5 Ways Hospital Billing Services Can Reduce Claim Denials
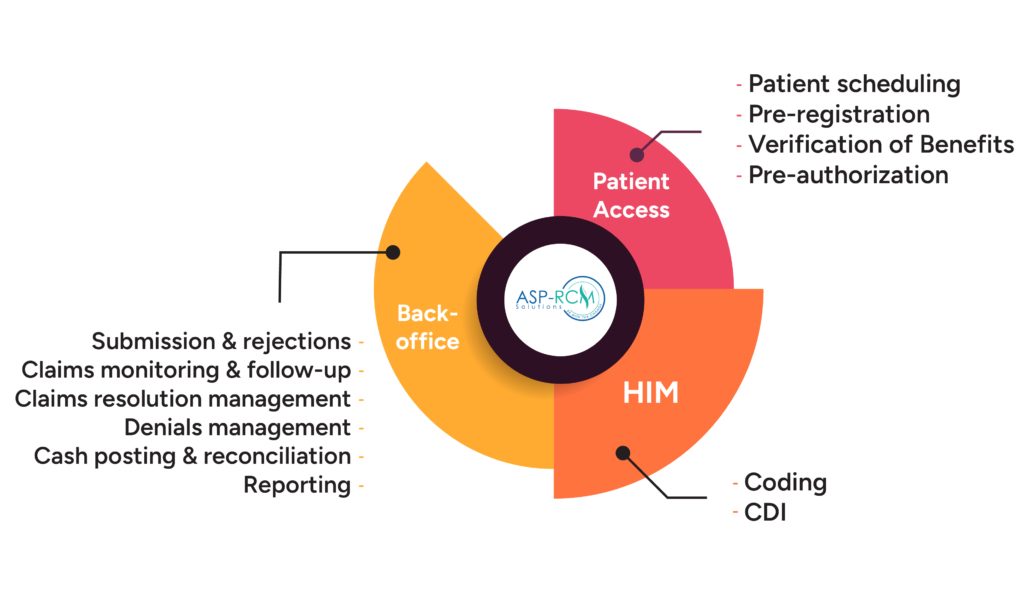
Claim denials are a major hurdle for healthcare providers, often leading to delayed payments, revenue losses, and administrative burden. For hospitals, where high patient volumes and complex billing codes are the norm, minimizing claim denials is critical for maintaining healthy cash flow and patient satisfaction. This is where professional hospital billing services come into play.
Hospital billing services specialize in managing the billing and claims process efficiently, ensuring that claims are submitted accurately, promptly, and in compliance with payer requirements. Below are five key ways hospital billing services can help reduce claim denials and boost revenue cycle performance.
1. Accurate Patient Data Collection and Verification
Many claim denials stem from simple errors at the front end of the billing cycle, particularly during patient registration. Incorrect or incomplete data—such as misspelled names, wrong insurance IDs, or outdated policy information—can trigger automatic rejections from insurance companies.
Hospital billing services are equipped with trained staff and automated systems to:
-
Verify insurance eligibility in real-time
-
Validate policy coverage for specific services
-
Confirm demographic and plan details before the patient receives care
By ensuring data accuracy from the beginning, billing services can significantly reduce the chances of denials caused by administrative oversights.
2. Proper Medical Coding and Documentation
One of the most common reasons for claim denials is improper coding. Coding errors—such as using outdated CPT/ICD codes, incorrect modifiers, or missing diagnosis-to-procedure links—can result in claims being rejected or underpaid.
Professional hospital billing services employ certified medical coders who:
-
Stay updated with the latest coding guidelines and payer-specific rules
-
Review medical documentation to ensure appropriate code assignment
-
Use software tools that flag potential coding errors before claim submission
With accurate and compliant coding, the likelihood of denials due to coding discrepancies is dramatically reduced.
3. Timely and Clean Claim Submissions
Delays in submitting claims or submitting incomplete ones—often referred to as “dirty claims”—are a leading cause of denials. Every payer has a specific time window within which a claim must be submitted; missing that window can mean forfeiting reimbursement altogether.
Hospital billing services follow best practices such as:
-
Establishing automated claim scrubbing to identify errors pre-submission
-
Using electronic claim submissions for faster processing
-
Tracking submission deadlines for each payer
Submitting clean claims in a timely manner not only lowers the risk of denials but also speeds up reimbursement cycles.
4. Proactive Denial Management and Follow-Up
Even with best practices in place, some claims may still get denied. What sets efficient billing services apart is their ability to track, analyze, and resolve those denials quickly.
Hospital billing services typically offer:
-
Real-time denial tracking dashboards
-
Root cause analysis of denied claims
-
Resubmission protocols for corrected claims
-
Appeals for unjustified denials
By acting quickly on denials and understanding their patterns, billing teams can prevent similar issues in the future and recover lost revenue more effectively.
5. Compliance with Changing Payer Regulations
Payers constantly update their billing and documentation requirements. Staying compliant with these changes is a challenge for in-house billing teams already burdened with daily operations.
Hospital billing services stay ahead by:
-
Monitoring payer bulletins and policy updates
-
Adjusting workflows and coding practices in response to changes
-
Training billing and coding staff on new requirements
This ongoing compliance ensures that hospitals are not caught off guard by new rules that could otherwise lead to avoidable denials.
Conclusion
Reducing claim denials is not just about fixing mistakes after they happen—it’s about building a proactive, accurate, and compliant billing process from start to finish. Hospital billing services offer the expertise, tools, and processes needed to minimize denials and maximize reimbursements.
By focusing on data accuracy, compliant coding, timely submissions, denial follow-up, and regulatory compliance, hospitals can achieve better financial outcomes and devote more resources to patient care.
If your hospital is facing a high denial rate or struggling with delayed reimbursements, investing in a reliable hospital billing service could be a smart and strategic move.